Introduction- People living with human immunodeficiency virus (HIV) infection (PLWH) are at increased risk for Hodgkin and non-Hodgkin lymphoma. Incidence of HIV-associated lymphoma fell dramatically after the introduction of combined antiretroviral therapy (cART) in the mid-1990s, and the distribution of lymphoma subtypes shifted away from those associated with severe immunosuppression. This study examines trends in the incidence and outcomes of HIV-associated lymphomas diagnosed and treated at an urban, minority-serving cancer center in the United States since 2000.
Methods- A retrospective cohort of patients diagnosed with or treated for HIV-associated lymphoma at University of Maryland Medical Center in Baltimore from 2000-2021 was identified and analyzed. Data from patients diagnosed with lymphoma from 2000-2013 was previously published. Data on patients diagnosed or treated for lymphoma at UMMC from 2014-2021 was abstracted from patients' electronic medical records. Data was summarized using simple descriptive statistics. Categorical variables were compared using Chi-squared tests.
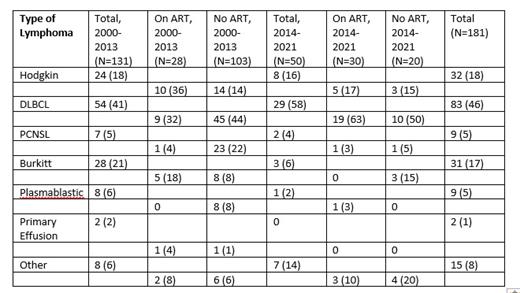
Results- The previously published study noted 160 patients with HIV-associated lymphoma during 2000-2013 (P1), of whom 131 had sufficient data for analysis. We identified 51 PLWH diagnosed with or treated for lymphoma at UMMC from 2014-2021 (P2), of whom 50 had sufficient data for analysis. The majority were male (73% during P1, 60% during P2) and African American (80% in P1, 76% in P2). Median age at diagnosis was 45 years in P1 and 42 years in P2. Median CD4 count at diagnosis was 104 cells/ul during P1 and 103 cells/ul (IQ range 35-194.5) during P2. PLWH not diagnosed with HIV prior to their lymphoma diagnosis remained similar (23% P1, 26% P2). The proportion of PLWH on cART at the time of lymphoma diagnosis increased over the course of the study period, from 28/131 (21%) to 30/50 (60%) during P2 (p<0.0001). Median Log 10 viral load (HIV-1 RNA copies/mL) was 4.7 during P1 and 2.7 during P2. Diffuse large B-cell lymphoma (DLBCL) was the most common type of lymphoma throughout the study period, representing 54 of 131 (41%) cases during P1 and 29 of 50 (58%) of cases during P2. Hodgkin lymphoma (HL) was the 2 nd-most common lymphoma, comprising 18% of cases during P1 and 16% during P2 (Table 1). The proportion of patients receiving some lymphoma treatment was 85% during P1 and 96% during P2, including 92% who received chemotherapy and/or monoclonal antibodies. Fourteen patients during P2 died prior to, during, or within eight weeks of completing 1st-line lymphoma treatment, including four deaths due to progressive lymphoma and six deaths due to infection. 54% of evaluable patients during P2 achieved a complete response (CR) to first-line treatment. 12-month overall survival (OS) was 49% during P1 and 61% during P2 (p=0.31). 24-month OS was 41% during P1 and 50% during P2 (p=0.44). Progression free survival (PFS) in P2 was 51% at 12 months and 42% at 24 months. For PLWH with DLBCL during P2, 56% achieved a CR to 1 st-line therapy; PFS was 49% at 12 months and 46% at 24 months. OS for this group was 62% at 12 months and 53% at 24 months. For all patients with DLBCL (with and without HIV) treated at our center from 2015-2019, 77% achieved CR to 1 st-line therapy, PFS was >61% at 24 months, and OS was >69% at 24 months. Three PLWH had perinatal acquisition of HIV and a mean age of 27 years at lymphoma diagnosis. 24-month OS for this group was 33%, compared to 51% for PLWH with other routes of transmission (p=0.78).
Conclusions- Patients with HIV-associated lymphoma during P2 were more likely to be on cART and had lower viral loads at time of lymphoma diagnosis than during P1, but had similarly low CD4 counts. Distribution of lymphoma subtypes was similar during the two periods, with DLBCL and HL most common. Outcomes remain poor, especially among those patients with low CD4 counts and detectable viremia at the time of diagnosis. Prolonged duration of HIV viremia or immune suppression, related to early acquisition of infection or intermittent or partial adherence to cART, may increase the risk of adverse lymphoma outcomes. Engaging and retaining patients in HIV care is essential to reducing mortality from HIV-associated lymphoma. HIV therapies that more quickly suppress viremia and promote rapid immune reconstitution might also improve lymphoma outcomes.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal